
Amaha / / / Understanding the Difference Between Psychosis and Neurosis: Science, Symptoms, Causes & Treatments
ARTICLE | 7 MINS READ
Understanding the Difference Between Psychosis and Neurosis: Science, Symptoms, Causes & Treatments
Published on
26th Sep 2025

Dr Divya G Nallur
MD Psychiatry

In India, where mental health stigma is still a huge hurdle, knowing the distinction between Psychosis and Neurosis is like having a secret key to understanding. A recent study by NIMHANS found that nearly 3.5% of the population suffers from neurosis-related issues, and a significant number of people experience psychotic symptoms, yet the treatment gap is a staggering 70-92%.
Dr. Khushboo Kansal, a leading psychiatrist at Amaha, Delhi, puts it beautifully: "The human mind is like a sophisticated orchestra. Neurosis is when a few instruments play slightly off-key, but the music continues. Psychosis is when the conductor loses touch with reality, and the entire symphony becomes disconnected from the audience."
The core distinction between psychosis and neurosis is about their grip on reality.

Connect with Experts dealing with Psychotic & Neurotic Disorders
93% Felt Better in 4+ Sessions after Amaha's Integrated Collaborative Care
What Exactly Are Psychosis and Neurosis?
Psychosis refers to a severe mental state where a person loses touch with reality. Hallucinations, delusions, and disorganised thinking are common symptoms of psychosis. Imagine feeling convinced of something others can’t see or hear.
Neurosis involves emotional distress like severe depression, anxiety, phobias, or obsessive behaviours while still knowing what’s real. Someone with neurosis may feel paralysed by constant worry, but they usually know their fears are exaggerated.
Neurosis involves emotional distress, anxiety, and irrational fears, but individuals maintain their grip on reality. They know something's wrong, even if they can't control their responses.
Psychosis, however, represents a fundamental break from shared reality. People experiencing psychosis may see, hear, or believe things that others don't perceive as real.
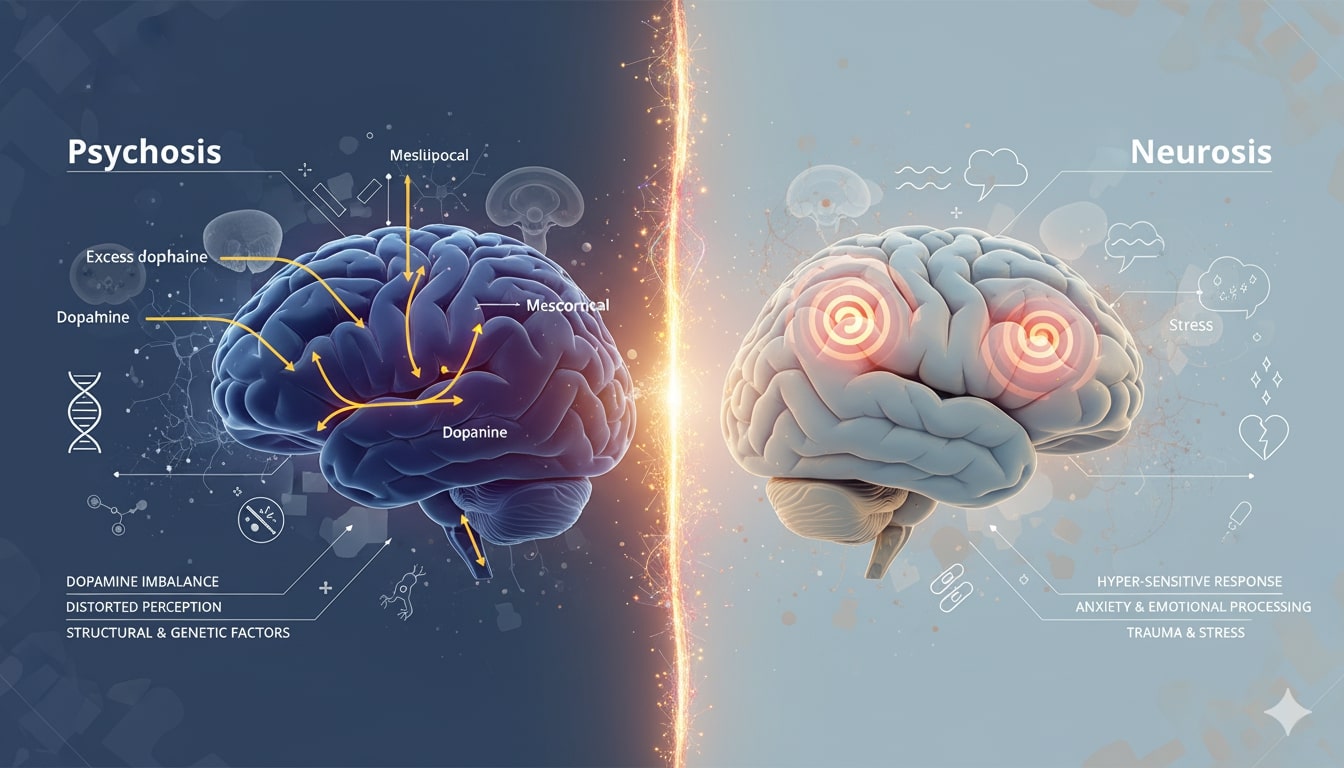
The Fascinating Neuroscience Behind Psychosis and Neurosis
Psychosis is often linked to disruptions in brain chemistry, particularly with the neurotransmitter dopamine. An excess or imbalance of dopamine can lead to the distorted perceptions and thought processes we see in psychosis. There are also structural and genetic factors at play. It's a physiological issue as much as it is a psychological one.
With neurosis, the picture is more about the psychological and emotional landscape. It often comes from unresolved trauma, persistent stress, or deep-seated internal conflicts. The brain is reacting to these stressors, leading to heightened activity in areas associated with anxiety and emotional processing, like the amygdala. It’s not a disconnect from reality, but a hyper-sensitive, often painful, response to it.
Recognising the Symptoms: Neurosis vs Psychosis
Symptoms of Psychosis
- Hallucinations (seeing, hearing, feeling things others don't)
- Delusions (fixed false beliefs)
- Disorganised thinking and speech
- Bizarre or inappropriate behaviour
- Loss of insight (not recognising symptoms as abnormal)
- Social withdrawal and functional decline
Symptoms of Neurosis
- Persistent Anxiety and Worry: Feeling on edge, restless, and constantly worried about things, big or small.
- Obsessive Thoughts and Compulsive Behaviours: Repetitive, unwanted thoughts and a need to perform certain rituals to relieve anxiety.
- Physical symptoms like racing heartbeat, sweating, or trembling, headaches, stomach issues, and chronic fatigue that have no clear medical cause.
- Phobias that seem irrational but feel very real
- Sleep disturbances and concentration problems
- Emotional outbursts or mood swings
The key difference? Someone with neurosis might say, "I think I'm going crazy," whilst someone in psychosis might say, "Everyone else is crazy; I'm the only one who sees the truth."
What Triggers These Conditions?
Causes of Psychosis
- Genetic vulnerability: Strong family history increases risk
- Brain chemistry: Imbalanced neurotransmitters, especially dopamine
- Substance abuse: Cannabis, alcohol, or synthetic drugs
- Medical conditions: Brain injuries, infections, or autoimmune disorders
- Severe stress: Major life events can trigger first episodes
Causes of Neurosis
- Childhood experiences: Overprotective parenting, trauma, or chronic stress
- Personality traits: Perfectionism, high sensitivity, or low self-esteem
- Life stressors: Job pressure, relationship issues, financial problems
- Genetic predisposition: Family history of anxiety disorders
- Cultural factors: In Indian society, academic pressure and arranged marriage stress often contribute
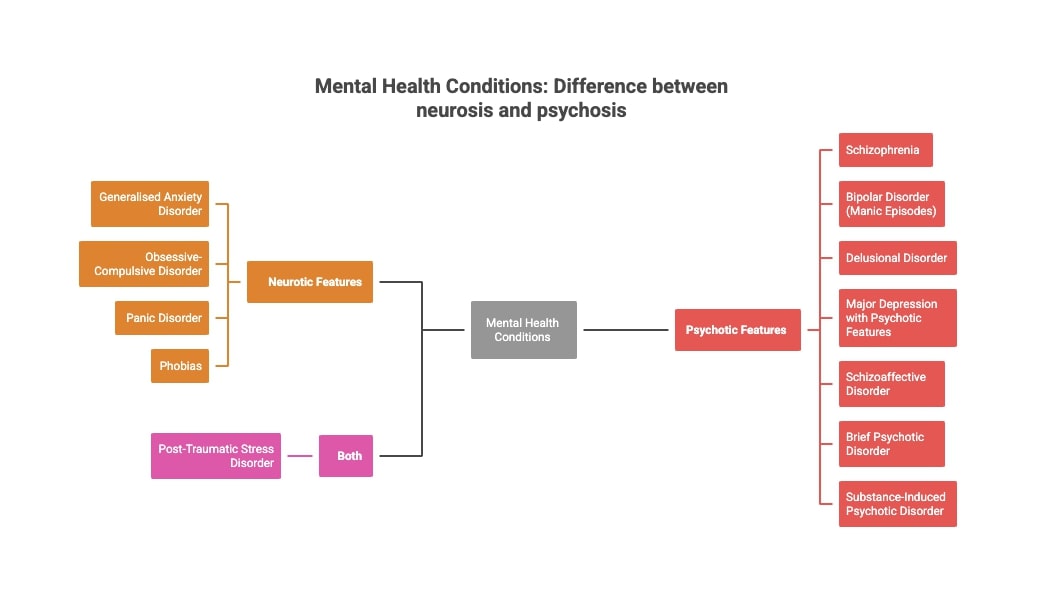
Can Someone Experience Both Neurosis and Psychosis?
Yes. It’s uncommon, but a person can present features of both. For example, someone might have generalised anxiety (neurosis) while also experiencing delusional episodes (psychosis). It makes diagnosis and treatment more complex, but not impossible.

Self-Assessment: Recognising the Signs of Psychosis & Neurosis
Psychosis Warning Signs Self-Assessment
- Have others mentioned that you're saying or doing strange things?
- Do you hear voices or see things others don't?
- Do you have strong beliefs that others find bizarre?
- Has your ability to work or maintain relationships declined significantly?
- Do you feel like people are plotting against you without clear evidence?
- Do you believe people are controlling or following you?
- Do your thoughts feel jumbled or disconnected?
Quick Neurosis Self-Check
- Do you worry excessively about everyday situations?
- Do physical symptoms (headaches, stomach issues, racing heart or constant fatigue) appear during stress?
- Do you avoid certain situations due to unreasonable fears?
- Are you aware that your worries might be excessive?
- Do you maintain normal relationships and work performance?
- Do you feel restless even when there’s no danger?
- Do you find yourself repeating habits to calm down?
- Have I been feeling sad, low, or unmotivated for a long time?
Important note: These aren't diagnostic tools. If you're concerned, consult a mental health professional immediately.
Mental Health Conditions - Different Psychosis and Neurosis conditions
Treatment Approaches & Support for Psychosis and Neurosis: Different Paths to Recovery
Treating Psychosis
Psychotic conditions require more intensive intervention:
- Antipsychotic medications are usually essential. Antipsychotic drugs work to balance the brain’s chemistry and reduce symptoms like hallucinations and delusions.
- Psychosocial interventions including family education, social skills training, and vocational rehabilitation help rebuild life skills.
- Hospitalisation might be necessary during acute episodes to ensure safety and stabilisation.
Treating Neurosis
- Psychotherapy remains the gold standard. Cognitive Behavioural Therapy (CBT) helps identify and change thought patterns. It's like having a personal trainer for your mind. Family therapy often helps, especially in Indian contexts where family dynamics significantly impact mental health.
- Medications like SSRIs or benzodiazepines can provide relief, but they're supporting actors, not the main hero of recovery.
- Lifestyle modifications work wonders: regular exercise, yoga, meditation, and proper sleep hygiene. These aren't just feel-good suggestions; they're evidence-based treatments.
How Therapy and Psychiatry Work Together
Therapy gives space to process fears and learn coping skills. Psychiatry steps in when medication and medical supervision are needed. In India, an integrated approach where therapists, psychiatrists, and families work together - has shown better outcomes.
Dr. Milan Balkrishnan, a renowned psychiatrist from Mumbai, explains: "In our culture, individual therapy often needs to become family therapy. We can't treat the person without understanding their family dynamics."
Why Early Intervention Matters
Early signs of psychosis or neurosis can look like “normal stress” or “quirky behaviour.” But waiting can worsen the illness, making treatment harder. Early help means better recovery, fewer relapses, and less stigma.
For psychosis, early intervention can be literally life-saving. Research shows that people who receive prompt treatment after first psychotic episodes have significantly better long-term outcomes. The brain's neuro-plasticity works in our favour when we act quickly.
In India, unfortunately, families often wait until symptoms become severe before seeking help. Cultural stigma and lack of awareness contribute to delayed treatment. But times are changing. More families now recognise that seeking help shows strength, not weakness.

Find out the Severity of your Symptoms
Take the Assessment to understand if you are Depressed or just Sad
Frequently Asked Questions:
Is neurosis a serious mental illness?
Neurosis involves distressing symptoms but maintains reality contact. While not as severe as psychosis, it significantly impacts quality of life and requires professional treatment for optimal recovery.
Can stress alone cause psychosis in healthy individuals?
Extreme stress rarely causes psychosis in mentally healthy people. However, it can trigger psychotic episodes in those with genetic vulnerability or underlying conditions like bipolar disorder.
Are neurotic people more intelligent than average?
Intelligence doesn't correlate with neurosis. However, highly intelligent individuals may overthink situations, potentially increasing anxiety. Neurosis affects people across all intelligence levels equally.
How long does psychosis last without treatment?
Untreated psychosis can persist for months or years, often worsening over time. Early intervention significantly improves outcomes. Some brief psychotic episodes resolve naturally within days to weeks.
Can yoga and meditation cure neurosis completely?
While yoga and meditation significantly help manage neurotic symptoms and reduce stress, they're best used alongside professional therapy rather than as standalone cures for clinical conditions.
How can I support a friend with neurosis or psychosis?
The best way is to be patient, non-judgmental, and understanding. Encourage them to seek professional help without pressuring them. Listen to them without trying to fix their problems, and help them find a professional who can provide expert care.
Can a person with psychosis be functional in society?
Absolutely. With the right combination of medication, therapy, and social support, many people with a history of psychosis live fulfilling lives. Treatment helps manage the symptoms, allowing them to work, maintain relationships, and pursue their passions.
Was This Article Helpful?
Yes
No



Build a good life for yourself
with Amaha
Best App
for Good
on Google Play India

Amaha is equipped to provide care and support for individuals experiencing severe psychological distress, including complex psychiatric disorders and other complex conditions. For those in need of more intensive care and daily support, we are launching an in-patient care facility in Bengaluru soon.
If you or someone you know is experiencing at-risk behaviors or safety concerns, or any other life-threatening crisis or critical mental health situation, contact a helpline or go to the nearest hospital or emergency room. Having a close family member or friend with you for support can be invaluable during this time.
For emergency mental health support, please call the national Tele MANAS helpline at 1-800 891 4416.