
Amaha / / / Anxiety vs Depression: Do I have Anxiety or Depression or both?
ARTICLE | 4 MINS READ
Anxiety vs Depression: Do I have Anxiety or Depression or both?
Published on
7th Jul 2025

Dr Divya G Nallur
MD Psychiatry

Recent studies show that nearly 200 million Indians struggle with mental health issues, with anxiety and depression being the most common culprits. But here's what's confusing many people: these two conditions often feel similar and are used interchangeably by many, yet they're fundamentally different.
Dr. Geethanjali, a leading psychiatrist from Mumbai explains "Anxiety and depression can coexist, mirror each other, or even mask one another, making it challenging for both patients and healthcare providers to distinguish between them."
That confusion is completely normal. I remember talking to my neighbour Ravi last month. He'd been feeling overwhelmed for weeks, couldn't sleep properly, and kept worrying about everything from his job to his family's health. "Am I anxious or depressed?" he asked me. Honestly, even I wasn't sure.
Reference: https://pmc.ncbi.nlm.nih.gov/articles/PMC10793817/

Are your symptoms affecting your daily life and those around you?
Speak to our Coach team to understand how you can get Better
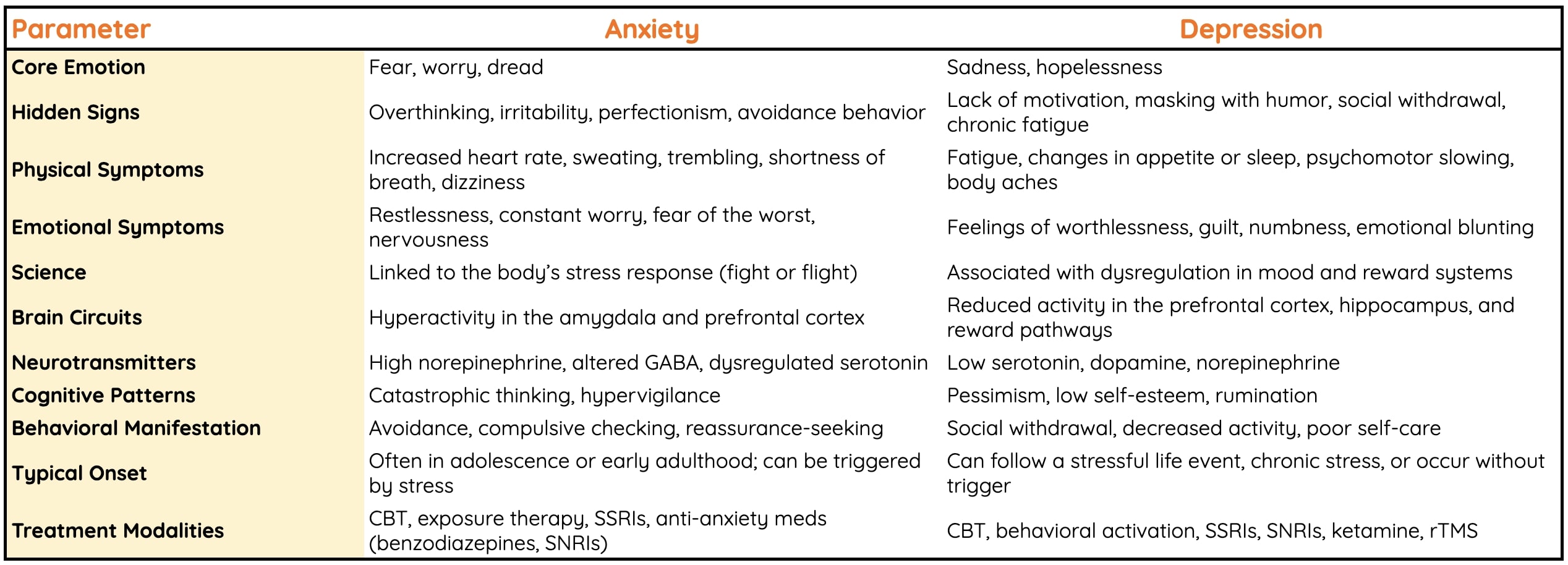
The Core Difference Between Anxiety and Depression
Anxiety is your mind's alarm system. It's that constant "what if" chatter that keeps you on edge about future events. Depression is more like a feeling that weighs you down making everything feel pointless and exhausting.
Anxiety is more about anticipation of future scenarios, worrying about potential threats or negative outcomes, often without a specific immediate danger which is triggered due to increased activity in the prefrontal cortex. Anxiety and fear are adaptive responses rooted in the brain’s emotional centers, especially the Limbic system, Amygdala, hippocampus, prefrontal cortex
Depression is a condition due to disturbances in 3 major neurotransmitters: Serotonin (regulates mood, sleep, and appetite), Dopamine (involved in motivation and reward), Noradrenaline (manages attention and arousal). Depression is linked to abnormal functionality in brain circuits involving the prefrontal cortex, anterior cingulate cortex, amygdala, hippocampus and striatum. These areas are crucial for regulating mood, motivation, emotional responses, cognitive control and self-reflection.
Think of it this way: anxiety makes you feel like you're running a marathon even when you're sitting still. Depression makes you feel like you can't even get out of bed to start the race.
But here's where it gets tricky. Sometimes these feelings overlap so much that you can't tell which one you're dealing with.
Anxiety Symptoms: When Your Mind is stuck creating future scenarios
Anxiety symptoms typically revolve around excessive worry and physical tension. Your body literally thinks there's danger everywhere, even when you're just sitting at home watching Netflix.
The most common anxiety symptoms include:
Physical signs: Heart pounding, sweating, trembling, shortness of breath, and those annoying muscle tensions that make your shoulders feel like concrete blocks.
Mental symptoms: Racing thoughts that jump from one worry to another. You might obsess over that presentation next week or convince yourself that headache is definitely something serious.
Behavioral changes: Avoiding social situations, constantly seeking reassurance from others, or checking things repeatedly. My cousin started avoiding family gatherings because she worried about saying something embarrassing.
Anxiety is future-focused. You're always bracing for something bad that might happen, even when logically you know it probably won't.
Depression Symptoms: When Everything Feels Heavy and Pointless
Depression symptoms are quite different from anxiety, though they can be just as debilitating. Where anxiety speeds everything up, depression slows everything down.
Emotional symptoms: Persistent sadness, emptiness, or hopelessness. It's not just feeling blue after a bad day; it's like someone dimmed the lights on your entire world.
Physical symptoms: Fatigue that doesn't improve with rest, changes in appetite (either eating too much or too little), and sleep problems. You might sleep for 12 hours and still feel exhausted.
Cognitive symptoms: Difficulty concentrating, making decisions, or remembering things. Simple tasks feel monumentally difficult.
Behavioral changes: Withdrawing from friends and family, losing interest in activities you once enjoyed, and struggling with daily routines.
Depression is more about the present and past. You feel stuck in a cycle of negative thoughts about yourself, your life, and your future.
Do I Have Anxiety or Depression or Both?
Research suggests that about 60% of people with anxiety also experience depression, and vice versa. Both conditions affect similar brain regions and neurotransmitters like serotonin and dopamine. Plus, dealing with chronic anxiety can be exhausting, leading to depressive symptoms. Similarly, the hopelessness of depression can trigger anxiety about the future.
Some telltale signs that you might have both:
You worry constantly about the future (anxiety) but also feel hopeless about it (depression). You have trouble sleeping because your mind races (anxiety), but you also feel too tired to get out of bed (depression). Social situations make you nervous (anxiety), but you also don't enjoy them anymore (depression). This condition where a person is suffering from anxiety and depression together is called “Dysthymia”.
Hidden but Subtle Differences that are difficult to spot
Let me share something that might help you understand the difference better. When my friend Priya was dealing with anxiety, she'd call me at 2 AM worrying about her job interview the next day. She'd run through every possible scenario, convinced something would go wrong.
When she later experienced depression, she stopped calling altogether. She didn't care about the interview anymore. Nothing seemed worth the effort.
Energy levels: Anxiety often comes with restless energy, like you're wound up too tight. Depression typically involves low energy and motivation.
Sleep patterns: Anxiety usually makes it hard to fall asleep because your mind won't quiet down. Depression might make you sleep too much or wake up very early and not be able to get back to sleep.
Appetite: Anxiety can suppress your appetite or make you stress-eat. Depression usually leads to significant changes in eating patterns, either overeating or undereating.
Physical sensations: Anxiety creates tension and restlessness. Depression often feels like heaviness or numbness.
When Anxiety and Depression Coexist
Having both anxiety and depression isn't uncommon in India, especially given our cultural pressures and expectations. The combination can create a particularly challenging situation where you're simultaneously worried about the future and hopeless about it.
This dual diagnosis often looks like:
Constant worry about disappointing family members while also feeling detached from family relationships. Panic about work performance combined with loss of interest in career advancement. Social anxiety mixed with social withdrawal.
What Triggers These Conditions?
Understanding your triggers can help you distinguish between anxiety and depression. Anxiety triggers are usually specific: upcoming exams, social events, work deadlines, or health concerns. Depression triggers tend to be more general: major life changes, relationship problems, chronic stress, or even seasonal changes.
In Indian families, common triggers include:
For anxiety: Marriage pressure, career expectations, financial responsibilities, and social comparisons.
For depression: Family conflicts, job loss, health issues, or feeling disconnected from cultural values.
Sometimes the same situation can trigger both. Job stress might make you anxious about performance while also making you feel hopeless about your career future.
Getting Help: What Actually Works
The treatment approaches for anxiety and depression overlap significantly, which is helpful if you're dealing with both. Therapy, particularly cognitive-behavioral therapy (CBT), works well for both conditions. It helps you identify and change negative thought patterns.
Medications like SSRIs can be effective for both anxiety and depression. However, what works varies greatly from person to person.
Lifestyle changes also play a crucial role. Regular exercise, adequate sleep, and stress management techniques like meditation or yoga can significantly improve both conditions.
Don't underestimate the power of talking to someone you trust. Whether it's a family member, friend, or professional counselor, sharing your feelings can provide immense relief.
Frequently Asked Questions -
Can I have both anxiety and depression at the same time?
Yes, it's quite common to have both conditions simultaneously. About 60% of people with anxiety also experience depression, and vice versa. This happens because both conditions affect similar brain regions and neurotransmitters. Having both is called comorbid anxiety and depression, and it requires comprehensive treatment addressing both conditions.
How do I know if I have anxiety or depression?
Anxiety typically involves excessive worry about future events, racing thoughts, and physical symptoms like rapid heartbeat and sweating. Depression involves persistent sadness, loss of interest in activities, fatigue, and feelings of hopelessness. Keep a mood journal for a week noting your symptoms, and consult a healthcare provider for proper diagnosis.
What's the main difference between anxiety and depression symptoms?
The key difference is focus and energy. Anxiety symptoms are future-focused with restless energy, racing thoughts, and worry about "what if" scenarios. Depression symptoms are present-focused with low energy, persistent sadness, and feelings of hopelessness. Anxiety makes you feel wound up; depression makes you feel weighed down.
Do anxiety and depression have the same treatment?
While there's overlap in treatments, the approach may differ. Both respond well to cognitive-behavioral therapy (CBT) and certain medications like SSRIs. However, anxiety might benefit more from exposure therapy and relaxation techniques, while depression might need more focus on behavioural activation and mood regulation strategies.
Is it normal to confuse anxiety and depression symptoms?
Absolutely. Many symptoms overlap, including sleep problems, difficulty concentrating, and changes in appetite. Both conditions can also trigger each other - chronic anxiety can lead to depression, and depression can cause anxiety about the future. This confusion is why professional diagnosis is important rather than self-diagnosis.
Was This Article Helpful?
Yes
No



Build a good life for yourself
with Amaha
Best App
for Good
on Google Play India

Amaha is equipped to provide care and support for individuals experiencing severe psychological distress, including complex psychiatric disorders and other complex conditions. For those in need of more intensive care and daily support, we are launching an in-patient care facility in Bengaluru soon.
If you or someone you know is experiencing at-risk behaviors or safety concerns, or any other life-threatening crisis or critical mental health situation, contact a helpline or go to the nearest hospital or emergency room. Having a close family member or friend with you for support can be invaluable during this time.
For emergency mental health support, please call the national Tele MANAS helpline at 1-800 891 4416.