
Amaha / / / How To Tell If Shortness Of Breath Is From Anxiety: Understanding Anxiety-Induced Shortness of Breath
ARTICLE | 6 MINS READ
How To Tell If Shortness Of Breath Is From Anxiety: Understanding Anxiety-Induced Shortness of Breath
Published on
1st Sep 2025

Dr Dean Creado
MD Psychiatry

Nearly 40% of Indians experience anxiety-related breathing difficulties at some point, yet most dismiss it as "just stress." Dr. Vani Kulhalli from Amaha, a leading psychiatrist from Mumbai, puts it perfectly: “The mind does not distinguish between a real threat or a perceived danger, so your mind cannot tell between a ferocious dog chasing you or the office deadline to send in your report, the mind can trick the body into believing it’s in danger, and one of the first signs is breathlessness.”
Understanding how to tell if shortness of breath is from anxiety can save you unnecessary panic attacks and hospital visits. So if you’ve ever caught yourself wondering how to tell if shortness of breath is from anxiety, you’re not alone. And it’s not “just in your head.” There’s actual science, medical terms, and practical ways to figure it out.
The Science Behind Anxiety-Induced Shortness of Breath: Dyspnea, Hyperventilation Syndrome
The medical term for “Shortness of breath due to anxiety” is anxiety-induced dyspnea (that's the fancy word for breathlessness) includes several conditions: hyperventilation syndrome, panic-induced dyspnea, and psychogenic dyspnea.

Check if your symptoms is due to Anxiety and not medical?
Find out the severity of all your anxiety-induced dyspnea symptoms
Why do you feel breathless during anxiety?
Anxiety flips your body into survival mode. Stress hormones trigger shallow, rapid breathing called hyperventilation that reduces carbon dioxide in the blood. This imbalance makes you feel like you can’t get enough air, even though oxygen levels are normal. It’s your brain misreading the situation, not your lungs failing.
When anxiety kicks in, your sympathetic nervous system activates, your body goes into “fight or flight” mode. Adrenaline surges. Your heart races. Breathing gets shallow.
During anxiety episodes, your brain releases stress hormones like adrenaline and cortisol. These chemicals trigger rapid, shallow breathing patterns. Your diaphragm tightens, chest muscles contract, and suddenly you feel like you're breathing through a straw. The body thinks it’s preparing to outrun a tiger, but in reality, you might just be preparing for a meeting or waiting for your exam results.
Spotting the Signs: Common Symptoms of Anxiety-Related Breathing Issues
- Sudden shortness of breath that appears in stressful situations
- A feeling of chest tightness without wheezing or cough
- Tingling in fingers or lips (a side effect of hyperventilation)
- Dizziness, light-headedness, or feeling like you might faint
- Racing thoughts, sweating palms, nausea, or feeling detached from reality
- Hands and feet getting cold suddenly in stressful situations
- Breathing improves after the stressful situation has passed through distraction or calming techniques
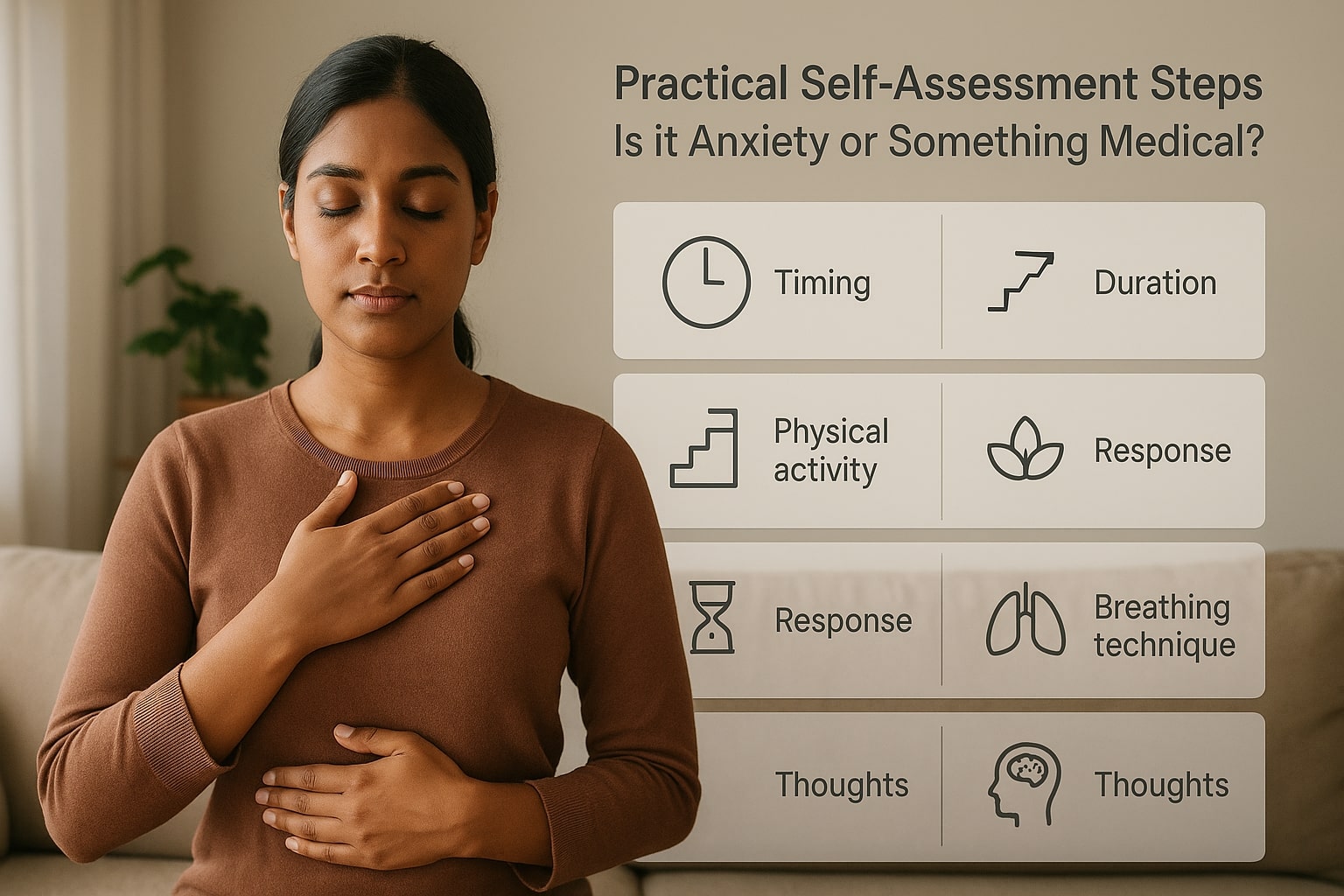
Practical Self-Assessment Steps - Self-check: Is it anxiety or something medical?
Here’s the tricky part. How do you know if shortness of breath is from anxiety and not from a medical condition like asthma, anaemia, or heart disease? A few practical pointers help:
1. Timing: If it happens only during stressful moments, anxiety is more likely.
2. Physical activity: If breathlessness worsens with walking or climbing stairs, it may be medical.
3. Duration: Panic-induced dyspnea usually lasts minutes, not hours.
4. Response: If calming techniques help, it’s likely anxiety-related.
5. Breathing technique: Check your breathing during episodes. Place one hand on your chest, another on your belly. During anxiety-induced breathing problems, your chest hand moves more than your belly hand. Normal breathing should primarily engage your diaphragm, making your belly rise and fall.
6. Pay attention to associated thoughts: Anxiety-induced dyspnea often comes with catastrophic thinking - "What if I can't breathe?" or "Something terrible is happening." Medical causes usually focus attention on physical sensations without the mental spiral.
Managing Shortness Of Breath From Anxiety
Once you know the culprit, management feels less scary. Here are simple ways to handle it:
- Slow breathing exercises: Count 4 seconds in, 6 seconds out.
- Grounding techniques: Look around and name 5 things you see to distract your mind.
- Regular exercise: Even a brisk 20-minute walk can balance breathing patterns.
- Progressive muscle relaxation: Start with your toes, tense them for 5 seconds, then release. Work your way up your body.
- Cognitive techniques: Remind yourself that anxiety-related breathing issues, while uncomfortable, aren't dangerous. Your body knows how to breathe.
- Limit caffeine and nicotine: They worsen anxiety symptoms.
Indian Practices for Regaining Control of your Breath
Indians have been dealing with anxiety long before psychiatry textbooks came along. Practices like Pranayama (controlled breathing), Nadi Shodhana (alternate nostril breathing), Bhramari pranayama (humming bee breath) and Shavasana (deep relaxation) have been known to calm both mind and body. Our ancestors understood the breath-mind connection long before modern psychology. Pranayama, the yogic science of breath control, offers powerful tools for managing anxiety-induced breathing problems.
These methods don’t just reduce anxiety-induced dyspnea, they also bring down overall stress levels
Professional Support & Guidance: How Therapy Transforms Breathing Patterns
Cognitive Behavioural Therapy (CBT) addresses the thought patterns that trigger breathing difficulties. Skilled therapists help you identify specific thoughts that precipitate episodes and develop alternative thinking patterns.
Exposure therapy gradually introduces anxiety triggers in controlled environments, helping you build confidence in managing symptoms. This approach particularly benefits people whose breathing issues occur in specific situations like crowded places or work presentations.
Acceptance and Commitment Therapy (ACT) teaches you to observe anxiety symptoms without fighting them. This mindful approach often reduces the secondary anxiety about breathing problems - the fear of fear itself that amplifies symptoms.
Many therapists also incorporate breathing retraining techniques, teaching you to recognise and correct dysfunctional breathing patterns. This combination of psychological and physiological approaches often provides lasting relief.
The Takeaway
Shortness of breath linked to anxiety is real, common, and manageable. Understanding the science, recognizing medical conditions like anxiety-induced dyspnea, knowing when it’s panic and not a lung condition, and applying practical tools—from breathing exercises to therapy can change how you respond the next time your chest feels tight.
So the next time you catch yourself thinking, “Why can’t I breathe properly? Am I ill?”—pause. It might just be your mind playing tricks. And the cure may already be in your breath.

Join Amaha's Community for learning to Cope with Anxiety
Get Daily Tips, Strategies and Advice
Frequently Asked Questions about Shortness of Breath due to Anxiety
How long should I try self-management techniques before seeing a doctor?
If you're confident your symptoms are anxiety-related and they respond to breathing techniques, you can manage them independently. However, see a healthcare provider if symptoms persist for weeks, occur during rest, worsen with activity, or if you develop new symptoms like chest pain, dizziness, or bluish lips.
What symptoms distinguish anxiety breathlessness from asthma or heart disease?
Anxiety-related breathlessness usually comes with tingling, dizziness, and a sense of “not getting enough air,” whereas asthma has wheezing and heart disease worsens with exertion.
Can pranayama completely cure anxiety-related breathing problems?
Pranayama is highly effective for managing anxiety-induced dyspnea and can significantly reduce episode frequency and intensity. However, it works best as part of a comprehensive approach that may include therapy, lifestyle changes, and sometimes medication. Regular practice builds resilience, but severe anxiety disorders often benefit from professional treatment alongside traditional practices.
Is hyperventilation syndrome the same as anxiety-induced shortness of breath?
Hyperventilation syndrome is one type of anxiety-related breathing problem characterised by rapid, shallow breathing that reduces carbon dioxide levels in your blood. However, anxiety can also cause other breathing patterns, including feeling unable to take deep breaths or chest tightness without hyperventilation.
Was This Article Helpful?
Yes
No



Build a good life for yourself
with Amaha
Best App
for Good
on Google Play India

Amaha is equipped to provide care and support for individuals experiencing severe psychological distress, including complex psychiatric disorders and other complex conditions. For those in need of more intensive care and daily support, we are launching an in-patient care facility in Bengaluru soon.
If you or someone you know is experiencing at-risk behaviors or safety concerns, or any other life-threatening crisis or critical mental health situation, contact a helpline or go to the nearest hospital or emergency room. Having a close family member or friend with you for support can be invaluable during this time.
For emergency mental health support, please call the national Tele MANAS helpline at 1-800 891 4416.