
Amaha / / / Depression: Signs and Symptoms
ARTICLE | 6 MINS READ
Depression: Signs and Symptoms
Published on
11th Jun 2025

Dr Anuradha Kabra
MD Psychiatry

Depression is a common mental health condition that can affect people of all ages, genders, and backgrounds. It is often associated with feelings of sadness, hopelessness, and low mood. However, depression can also have physical symptoms that are just as distressing and disruptive. Let’s explore some of the physical symptoms of depression and why it is important to recognize them.
What is Depression?
Depression is more than just feeling sad. It's a complex mental health disorder characterized by persistent feelings of sadness, loss of interest or pleasure in activities, and a range of emotional and physical problems. It is okay to feel sad when experiencing a major loss or a negative life event. But, unlike sadness, depression is an ongoing condition that can interfere with daily life, work, relationships, and overall quality of life.
Types of Depression
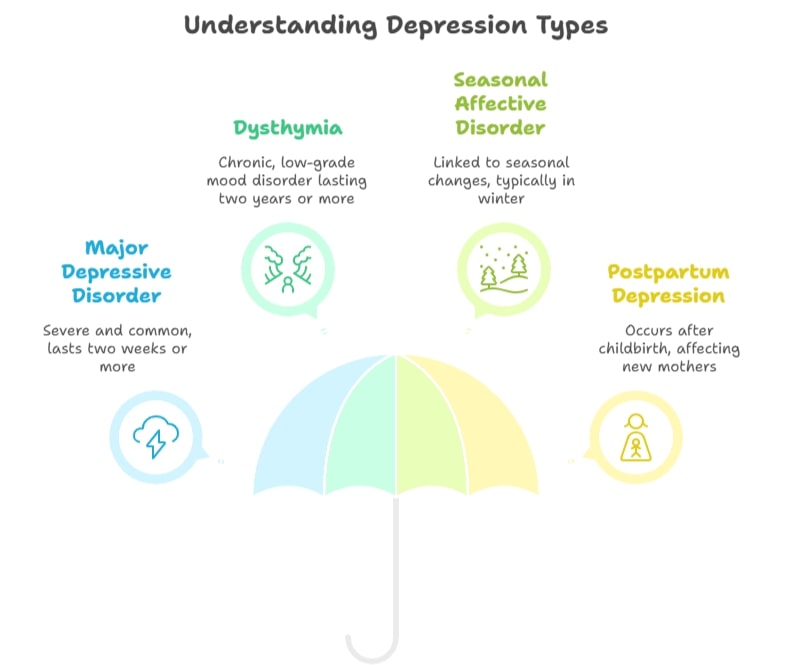
“Depression manifests in various forms, each with its specific diagnostic criteria and characteristics”, says Dr. Milan Balakrishnan, a psychiatrist at Amaha.
Understanding these types can help in accurate diagnosis and effective treatment.
Major Depressive Disorder (MDD): This is the most severe and common form of depression, characterized by a persistent depressed mood or loss of interest in activities, along with at least four other symptoms for two weeks or more.
Dysthymia: This type involves a chronic, low-grade depressed mood that lasts for at least two years. While the symptoms may not be as severe as MDD, they are persistent and can significantly impact a person's life.
Seasonal Affective Disorder (SAD): SAD is a type of depression that is linked to changes in seasons, typically beginning and ending at about the same times every year. Symptoms usually appear during the late fall or early winter months and go away during spring and summer.
Postpartum Depression (PPD): This type of depression occurs after childbirth, affecting new mothers. It involves more severe, long-lasting symptoms that can interfere with a mother’s ability to care for her baby and herself.
What Is The Difference Between Depression And Chronic Depression?
Signs and Symptoms of Depression
Here are some commonly experienced signs and symptoms. It's important to note that the symptoms listed below should be present for most of every day for a specified duration to meet diagnostic criteria.
- Persistent low mood: This is a pervasive feeling of sadness, emptiness, or hopelessness, often described as feeling "down in the dumps" for no apparent reason.
For instance, Sarah, a usually energetic and dynamic person found herself in a severely low mood with constant pessimism and difficulty in meeting people and socializing – something she really enjoyed and looked forward to earlier.
- Overwhelming negative thoughts: A depressed individual might feel like they are in a void with their minds being inclined to perceive things negatively, using absolute terms like 'never' or 'always' when describing events or situations. It becomes increasingly difficult to hold on to anything optimistic. These negative thought patterns can be self-perpetuating, making it difficult to break free without intervention.
- Almost no or less interest or pleasure in activities (Anhedonia): Once enjoyable activities, such as practicing a hobby, socializing, or spending time with loved ones, no longer bring satisfaction or interest.
- Significant weight loss, poor appetite, weight gain: Changes in body weight or appetite that are not due to dieting. Some people lose interest in food, while others may overeat as a coping mechanism.
- Insomnia or hypersomnia: Difficulty falling asleep, staying asleep, or waking up too early (insomnia), or conversely, excessive sleeping even during the day (hypersomnia).
For example, Arjun, a usually athletic and punctual individual found himself unable to sleep, even though he was exhausted. He spent his nights staring at the ceiling with constant anxious thoughts. Even when he managed to sleep away, he woke up in some time, feeling exhausted and drained. (Insomnia)
On the other hand, Sam always felt he wanted to sleep more even after getting 10-15 hours of sleep daily. He woke up tired, and dozed off in the afternoon, missing on plans and other daily routine activities. (Hypersomnia)
- Psychomotor retardation or agitation: Observable slowing of movements, speech, and thought processes, or restlessness, pacing, and inability to sit still.
During her deepest low moments, Isha felt like she had to make deliberate lip movements to speak. She felt her movements were very difficult to make and simple tasks like taking a bath seemed very effortful. (Psychomotor retardation)
Lilly, however, felt extremely restless accompanied by constant pacing, racing thoughts, and difficulty sitting in one place for too long. (Agitation)
- Fatigue or loss of energy: Feeling tired and lacking energy even after sufficient rest, making daily tasks feel overwhelming.
- Feelings of worthlessness or excessive guilt: Persistent negative self-perception, feeling inadequate, or guilty about things that are not one's fault.
- Diminished ability to think or concentrate, or indecisiveness: Difficulty focusing, remembering things, or making even simple decisions.
- Suicidal thoughts: Recurrent thoughts of death, suicidal ideation, or attempt. These are serious symptoms that require immediate professional attention.
Read more:
Dr Ahmed Reshamvala, a psychiatrist at Amaha, emphasizes, “The signs and symptoms of depression vary from person to person and can range in severity.”
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) outlines specific criteria for diagnosing depressive episodes.
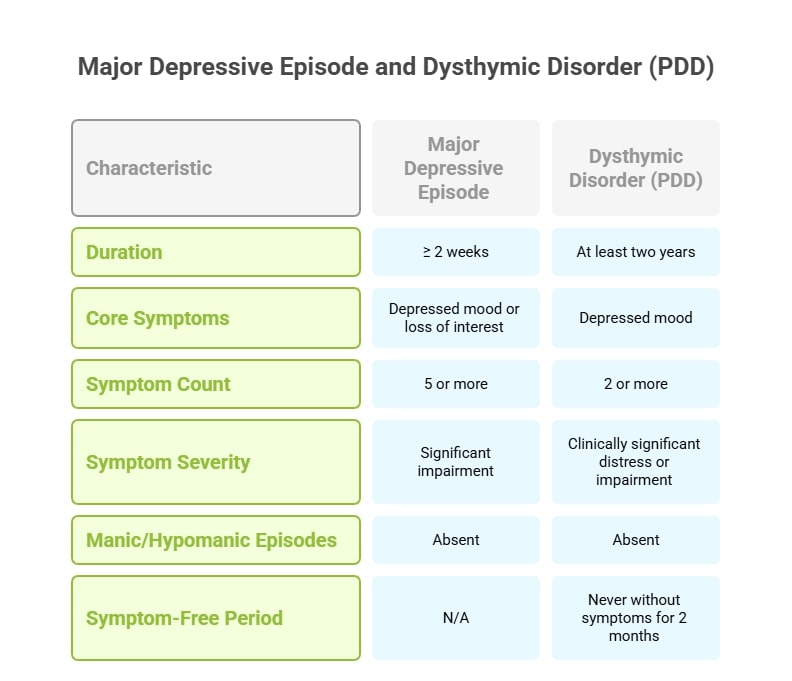
Major Depressive Episode
- 5 or more depressive symptoms for ≥ 2 weeks: A significant shift from previous functioning is observed.
- Must have either a depressed mood or loss of interest/pleasure: These are considered the core symptoms of depression.
- Symptoms must cause significant distress or impairment: The symptoms interfere with daily life, work, school, or relationships.
- No manic or hypomanic behavior: This distinguishes major depressive disorder from bipolar disorder.
Dysthymic Disorder (Persistent Depressive Disorder):
- Depressed mood for most of the time for at least two years: A chronic, persistent low mood.
- Presence of 2 or more symptoms of dysthymia: Less severe symptoms than major depression, but long-lasting.
- Never without symptoms for 2 months or more over 2 2-year periods: The symptoms are consistent and rarely remit.
- Symptoms must cause clinically significant distress or impairment: Despite being milder, the symptoms still affect daily functioning.
- No major depressive disorder in the first two years, no manic, hypomanic, or mixed episodes: This differentiates it from other mood disorders.
Read more: Understanding Treatment-Resistant Depression: Exploring Alternative Therapies
Signs and Symptoms of Depression in Women
Women are diagnosed with depression at nearly twice the rate of men. This could be due to hormonal fluctuations, societal pressures, and differing coping mechanisms. Symptoms can include:
- Increased feelings of guilt and self-blame: Women may internalise problems and blame themselves.
- More pronounced feelings of sadness, worthlessness, and helplessness: These emotional symptoms may be more prominent.
- Changes in appetite and weight: More likely to experience increased appetite and weight gain.
- Higher rates of atypical depression: This involves mood reactivity (mood improves in response to positive events), increased appetite, weight gain, and hypersomnia.
- Physical symptoms like headaches, stomach problems, and chronic pain: These can be common and may be dismissed as unrelated to depression.
- More likely to experience seasonal affective disorder (SAD): The cyclical nature of hormones may play a role.
Signs and Symptoms of Depression in Men
Depression in men can often be overlooked or misdiagnosed because they may express symptoms differently due to societal expectations of masculinity. They might internalise emotions or express them as irritability rather than sadness.
- Irritability, anger, and aggression: Instead of sadness, men may display increased agitation and anger.
- Escapist behaviour: Engaging in risky behaviours, excessive drinking, drug use, or reckless driving.
- Workaholism: Burying themselves in work to avoid dealing with emotions.
- Fatigue, loss of interest in hobbies, and sleep disturbances: These physical and behavioural symptoms may be more noticeable.
- Physical aches and pains: Men may report more physical complaints as a way to express distress.
- Difficulty expressing emotions: May be reluctant to talk about their feelings of sadness or vulnerability.
- Higher rates of suicide: Despite lower diagnosis rates, men have a higher suicide rate than women.
Signs and Symptoms of Depression in the Elderly
Depression in older adults is often underdiagnosed because symptoms can be mistaken for normal ageing, medical conditions, or medication side effects.
- Persistent sadness, anxiety, or low mood: May not verbalise sadness as readily.
- Loss of interest in hobbies or social activities: Withdrawal from activities they once enjoyed.
- Memory problems or difficulty concentrating: Often mistaken for dementia.
- Physical aches and pains: Somatic complaints without a clear cause.
- Sleep disturbances: Insomnia or waking up frequently.
- Loss of appetite or weight loss: This can lead to nutritional deficiencies.
- Neglect of personal care: Poor hygiene or living conditions.
Signs and Symptoms of Depression in Teens
Adolescence is a period of significant emotional and physical changes, making it challenging to differentiate typical teenage moodiness from depression.
- Irritability, anger, or hostility: More common than overt sadness in teens.
- Withdrawal from friends and family: Isolating themselves from social interactions.
- Changes in academic performance: A sudden drop in grades or a lack of interest in school.
- Loss of interest in activities: Giving up on sports, hobbies, or clubs they once loved.
- Changes in sleep patterns: Excessive sleeping or insomnia.
- Changes in appetite or weight: Eating more or less than usual, leads to weight fluctuations.
- Frequent complaints of physical ailments: Headaches, stomachaches, or other unexplained pains.
- Feelings of worthlessness or guilt: Low self-esteem and self-blame.
- Reckless behaviour: Engaging in risky activities, substance abuse, or self-harm.
Suicidal thoughts or attempts: Recurrent thoughts of death, suicidal ideation or attempt.

Take a Quick Mood Check
Not sure if it's just sadness or something deeper? Take this assessment to understand your emotional state in just a few minutes.
Signs and Symptoms of Postpartum Depression
Postpartum depression (PPD) is a serious mood disorder that can occur in women after childbirth..
- Tiredness after labour and delivery: Beyond normal fatigue, feeling utterly drained.
- Overwhelmed with a new baby: Feeling unable to cope with the demands of motherhood.
- Crying all the time, often for no reason: Frequent and uncontrollable crying spells.
- Severe anger and crankiness: Increased irritability and short temper.
- Loss of pleasure: Inability to find joy in activities, including interacting with the baby.
- Feelings of worthlessness, hopelessness, and helplessness: Profound negative self-perceptions.
- Thoughts of death or suicide: Serious thoughts that require immediate medical attention.
- Thoughts of hurting someone else: Particularly concerning if directed towards the baby.
- Trouble concentrating or making decisions: Brain fog and indecisiveness.
Read more: Common Myths About Postpartum Depression
Physical Signs and Symptoms of Depression
Physical symptoms of depression are not simply in your head. They are real, physical manifestations of a mental health condition that can have a significant impact on daily life and well-being.
Fatigue and Low Energy
One of the most common physical symptoms of depression is persistent fatigue and low energy. People with depression may feel exhausted and run down, even after a seemingly good night's sleep. They may find it incredibly difficult to get out of bed in the morning or may struggle to keep up with their usual activities and responsibilities. This pervasive fatigue can also be accompanied by a lack of motivation and interest in things that once brought joy, making even simple tasks feel monumental.
Physical Pain
The brain and body are deeply connected, and emotional distress can manifest physically. Some people with depression may also experience severe or chronic pain, which can further contribute to feelings of hopelessness and helplessness. One may also experience psychosomatic pain, which is a type of pain that is caused or exacerbated by psychological factors, such as emotional distress, rather than solely physical injury or disease. In individuals with depression, chronic stress, anxiety, and muscle tension can contribute to persistent headaches, back pain, and widespread body aches.
Digestive Issues
The gut-brain axis is a well-established connection, and depression can significantly affect the digestive system, leading to symptoms such as nausea, constipation, and diarrhoea. This can be due to changes in the brain's regulation of the digestive system, altered gut microbiome, and a reduction in appetite and food intake.
Sleep Disturbances
Sleep disturbances are another common and often debilitating physical symptom of depression. People with depression may find it difficult to fall asleep (insomnia), stay asleep (frequent waking), or wake up feeling refreshed and rejuvenated. Some individuals may experience hypersomnia, sleeping excessively but still feeling tired.
Appetite Changes
Depression can also cause significant changes in appetite. Some people may experience a marked loss of appetite and subsequent weight loss, finding food unappealing or even difficult to swallow. Others may experience increased appetite, leading to overeating and weight gain, often using food as a source of comfort or distraction from their emotional pain.
Sexual Dysfunction
Depression can significantly impact sexual health, causing sexual dysfunction such as decreased libido (sex drive), erectile dysfunction in men, or difficulty reaching orgasm in both men and women. This can be due to changes in hormone levels, neurotransmitter imbalances in the brain, as well as a general decrease in interest in physical activity and intimacy due to low mood and energy. Sexual dysfunction can also contribute to feelings of low self-esteem, shame, and isolation, further compounding the emotional burden of depression.
If you are experiencing any of these symptoms, whether emotional or physical, it is important to seek help and support from a mental health professional. Early intervention can improve outcomes and help individuals navigate through depression.
Read more about What to Do When Depression Becomes Overwhelming?
Navigating Through Depression: Caregiver and Loved Ones Support
Supporting someone with depression can be challenging, but your role as a caregiver or loved one is invaluable.
- Learn about depression, its symptoms, and treatment options. Understanding what your loved one is going through can help you respond with empathy and patience.
- Create a safe space for them to express their feelings without fear of being judged or dismissed. Simply listening can be incredibly validating. Avoid offering unsolicited advice unless asked.
- Recovery from depression is a process, not an event. There will be good days and bad days. Avoid putting pressure on them to "snap out of it."
- Understand that you cannot "cure" their depression. Your role is to support them in their journey towards recovery.
- Encourage them to maintain social connections, even if it's just a short visit or phone call. Offer to facilitate these interactions.
- If your loved one expresses suicidal thoughts or intentions, take them seriously and seek immediate professional help. Do not leave them alone.
- Make sure to prioritise your well-being, seek support for yourself if needed, and practice self-care. You cannot pour from an empty cup.
- Acknowledge and praise any small progress they make, no matter how insignificant it may seem. This can boost their morale and give them hope..
Remember, depression is a serious illness, but it is treatable. With the right support and professional help, individuals can recover and lead fulfilling lives.

Talk to a Mental Health Expert
Feeling depressed or stressed? Talk to a expert who’ll listen, guide you, and help you feel better—one step at a time.
Frequently Asked Questions (FAQ)
1. What's the difference between feeling sad and having depression?
Sadness is a natural, temporary feeling in response to difficult situations and usually passes with time. Depression is a medical condition where deep sadness, emptiness, or hopelessness lasts for weeks or longer and affects daily life, relationships, and work.
2. How many symptoms do I need to have to be diagnosed with depression?
Doctors look for at least five symptoms lasting most of the day, nearly every day, for at least two weeks. One must be either a low mood or a loss of interest in things you used to enjoy. These symptoms must make daily life harder.
3. Why do men and women experience depression differently?
Women are diagnosed more often and may feel more sadness, guilt, or physical symptoms. Men might show depression through anger, irritability, or risky behaviors and may avoid talking about their feelings. These differences are due to hormones, social pressures, and coping styles.
4. Can depression cause physical symptoms?
Yes. Depression often leads to physical problems like constant tiredness, aches and pains, stomach issues, sleep troubles, and appetite changes. These are real and common.
5. How can I tell if a teenager has depression versus normal moodiness?
Teen depression is more than mood swings. Watch for ongoing irritability, withdrawal from friends, drop in grades, loss of interest in activities, big changes in sleep or eating, frequent physical complaints, or talk of self-harm.
6. What should I do if someone I know is having suicidal thoughts?
Take it seriously. Stay with them, contact a mental health professional or suicide hotline, and don’t try to manage it alone. Listen with care and never dismiss their feelings.
7. How can I best support someone with depression?
Learn about depression, listen without judgment, be patient, encourage professional help, and care for your own well-being too. Celebrate small steps forward and remember your support matters.
Was this article helpful?
Yes
No
If you didn't find what you were looking for, please reach out to us at [email protected] or +912071171501. We're here for you - for anything you might need.



Build a good life for yourself
with Amaha
Best App
for Good
on Google Play India

