
Amaha / / / When Sleep Holds You Hostage: Understanding Sleep Paralysis
ARTICLE | 6 MINS READ
When Sleep Holds You Hostage: Understanding Sleep Paralysis
Published on
4th Nov 2025

Dr Aruna Sri Sikha
MD Psychiatry

Imagine waking up but finding yourself completely frozen. Your eyes can move, you're fully conscious, but your limbs refuse to budge. Sometimes, there are shadowy figures in the room or a crushing weight on your chest.
Dr Anjali Mehta, a consultant psychiatrist at Mumbai's leading sleep clinic, says: "Sleep paralysis isn't a sign of madness or supernatural interference. It's your brain and body having a brief communication glitch, like a video call that freezes mid-conversation."
What causes sleep paralysis, and more importantly, how do we address it without dismissing someone's genuine fear? Let’s discuss in this article.
What Is Sleep Paralysis?
Sleep paralysis is a temporary inability to move or speak that occurs when you're waking up or falling asleep. It typically lasts from a few seconds to a couple of minutes, though it feels much longer when you're going through it.
Your mind is awake. Your body isn't. That's the simplest way to understand it.
During these episodes, people often report:
- Complete muscle immobility (except for eye movements and breathing)
- A sense of pressure on the chest
- Difficulty breathing or feeling suffocated
- Hallucinations (visual, auditory, or tactile)
- Intense fear or dread
The medical term for these episodes is "sleep paralysis," and whilst it's deeply unsettling, it's generally harmless. But just one experience of sleep paralysis can create anxiety around sleep, which in turn can impact how you feel and function throughout the day.

Get 15% OFF on First 3 Sessions - Use Code: FIRST15
Therapy works best when it’s approached with consistency. Take those first few steps with confidence, so you can begin your mental health journey. **Limited Period Offer
The Underlying Mechanism: Why Does It Happen?
- When you sleep, your brain cycles through different stages. REM (Rapid Eye Movement) sleep is when most vivid dreaming happens. During REM, your brain essentially paralyses your muscles to prevent you from acting out dreams.
- Sleep paralysis occurs when there's a disconnect in this process. Your consciousness wakes up, but your body's still in that paralysed REM state.
- The hallucinations happen because your dream state overlaps with waking consciousness. Your brain's still producing dream imagery whilst you're awake enough to process it as "real." That shadowy figure isn't actually there; it's your mind trying to make sense of the paralysis by creating a narrative around it.
Major Causes And Risk Factors
What causes sleep paralysis varies from person to person, but researchers have identified several contributing factors.
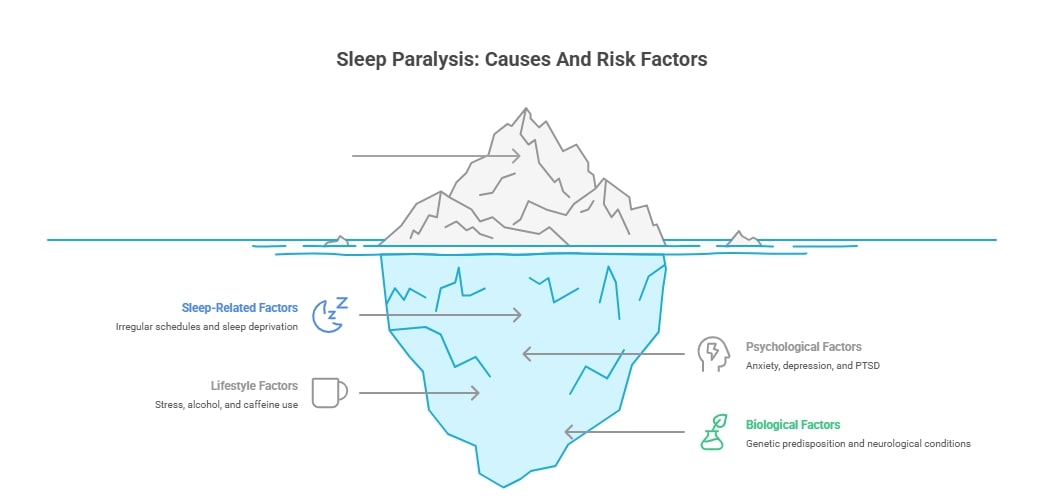
Sleep-Related Factors
Irregular sleep schedules top the list. In urban India, particularly in cities like Bengaluru, Mumbai, and Delhi, people often sleep past midnight and wake early for work. This chronic sleep deprivation disrupts your REM cycles.
Night shift workers are especially vulnerable. A software engineer working the US shift in Pune, for instance, might sleep during the day when their body's circadian rhythm expects wakefulness. This confusion between internal clocks and external schedules creates perfect conditions for sleep paralysis.
Sleep deprivation itself is massive. Getting less than six hours regularly doesn't just make you tired; it messes with how your brain manages sleep stages. When you finally do sleep properly, your brain tries to "catch up" on REM sleep, sometimes overshooting and causing these episodes.
Sleeping on your back (supine position) also increases risk. Many people notice their episodes only happen in this position, though scientists aren't entirely sure why.
Psychological & Mental Health Factors
Anxiety and depression frequently accompany sleep paralysis. It's a bit of a chicken-and-egg situation: does anxiety cause sleep paralysis, or does experiencing sleep paralysis create anxiety? Probably both.
Post-traumatic stress disorder (PTSD) shows particularly strong links. The hypervigilance associated with PTSD can interfere with normal sleep transitions, making episodes more likely.
Bipolar disorder and panic disorder also correlate with higher rates. The stress hormones these conditions produce can disrupt sleep architecture.
Here's something interesting: in India, where mental health stigma still runs deep, many people suffering from anxiety or depression don't seek help. They might experience recurrent sleep paralysis as an untreated symptom, never making the connection between their mental state and these frightening episodes.
Lifestyle & Substance Use
Stress deserves its own paragraph. Indian society, with its academic pressures, familial expectations, and competitive work environments, breeds chronic stress. Students often experience sleep paralysis during high-stress periods.
Alcohol and certain medications interfere with sleep quality. That evening drink might help you fall asleep initially, but it fragments your REM sleep later in the night.
Caffeine consumption late in the day can also contribute. Stimulants don't just delay sleep; they affect how smoothly you transition between sleep stages.
Genetic or Other Biological Factors
Sleep paralysis sometimes runs in families, suggesting genetic predisposition. If your parent experienced it, you're more likely to as well.
Certain neurological conditions increase risk, including narcolepsy (where sleep paralysis is actually a diagnostic criterion). Some research also points to disrupted neurotransmitter function, particularly involving GABA and serotonin.

Are You Sleeping Well? Find Out in Minutes
Take our quick sleep assessment to understand your sleep patterns and identify what might be affecting your rest. Gain insights and take the first step toward better, healthier sleep.
Why Are Some Cases Recurrent Or Severe?
Most people experience sleep paralysis occasionally. But for some, it becomes frequent enough to cause genuine distress.
Recurrent isolated sleep paralysis (RISP) is the medical term when episodes happen regularly without an underlying sleep disorder like narcolepsy. These cases often involve multiple risk factors compounding each other: poor sleep hygiene plus anxiety plus irregular schedules, for instance.
The fear itself can become a trigger. If you've had a terrifying episode, anxiety about sleeping can worsen your sleep quality, which then increases the likelihood of another episode. It's a vicious cycle.
Prevention & Management Strategies
Improve sleep hygiene first. This means:
- Maintaining consistent sleep and wake times
- Creating a dark, cool, quiet sleeping environment
- Avoiding screens an hour before bed
- Not sleeping on your back if that's when episodes occur
Address underlying mental health concerns. Therapy for sleep paralysis often means treating the anxiety or depression fuelling it. Cognitive Behavioural Therapy (CBT) has shown effectiveness, particularly CBT specifically designed for sleep issues (CBT-I).
Psychiatry for sleep paralysis might involve medication when psychological factors are significant. Selective serotonin reuptake inhibitors (SSRIs), which suppress REM sleep, sometimes help reduce episodes in severe cases. However, medication isn't typically the first line of treatment.
Stress management techniques make a real difference. Meditation, yoga and progressive muscle relaxation can all improve sleep quality.
During an episode itself, try to:
- Focus on moving small body parts first, like fingers or toes
- Concentrate on your breathing
- Remind yourself it's temporary and will pass
Some people find that trying to move their eyes or facial muscles helps break the paralysis faster.
Myths, Cultural Interpretations & When To Worry
Whilst respecting cultural beliefs, it's crucial to understand the medical reality. Sleep paralysis isn't possession; it isn't a curse, and no amount of holy water or talismans will address the underlying sleep disorder.
See a doctor if:
- Episodes happen frequently (more than once a week)
- They're severely impacting your sleep quality or daily functioning
- You're excessively sleepy during the day (could indicate narcolepsy)
- Episodes started after a head injury
- You're experiencing other concerning symptoms
A sleep specialist can rule out other sleep disorders and provide targeted treatment.
Finding Relief & Moving Forward
For many, simple lifestyle changes suffice. Better sleep habits, reduced stress, and perhaps changing sleeping position can dramatically reduce episodes. For others, particularly those with underlying mental health conditions, professional help makes all the difference.
People around you dismiss it as "just a bad dream" or worse, as weakness. But thousands of Indians experience this. You're not alone, you're not going mad, and with the right approach, you can reduce or eliminate these episodes.
Sweet dreams are possible again.

Overcome Sleep Struggles with Expert Guidance
Struggling with sleep paralysis or restless nights? Talk to our mental health coaches for personalised support and practical tools to improve your sleep and peace of mind.
Frequently Asked Questions
Q: What is sleep paralysis, and is it dangerous?
Sleep paralysis is a temporary inability to move or speak whilst falling asleep or waking up. Whilst terrifying, it's generally not dangerous. Your breathing continues normally, and the episode passes within minutes. However, if episodes are frequent or accompanied by excessive daytime sleepiness, consult a sleep specialist to rule out underlying conditions like narcolepsy.
Q: What causes sleep paralysis, and why do some people get it more than others?
Multiple factors cause sleep paralysis, including irregular sleep schedules, sleep deprivation, sleeping on your back, anxiety, depression, and stress. Some people are genetically predisposed. In India, factors like night shifts, exam stress, and irregular lifestyles contribute significantly. Those with anxiety disorders or PTSD experience it more frequently.
Q: Can sleep paralysis be cured permanently?
Whilst there's no single "cure," most people can significantly reduce or eliminate episodes through lifestyle changes: maintaining consistent sleep schedules, improving sleep hygiene, managing stress, and treating underlying mental health conditions. Therapy for sleep paralysis, particularly Cognitive Behavioural Therapy, helps many people. In some cases, psychiatry for sleep paralysis involving medication may be recommended.
Q: Why do I see scary figures or feel pressure on my chest during sleep paralysis?
These hallucinations occur because your brain is partially in a dream state whilst you're conscious. Your mind tries to explain the paralysis by creating narratives, often manifesting as shadowy figures or sensations of pressure. The "chest pressure" happens because you're trying to breathe with voluntary muscles whilst they're in REM atonia (temporary paralysis). It's frightening but not physically harmful.
Q: Is sleep paralysis related to mental health problems?
Yes, there's a strong connection. Anxiety, depression, PTSD, and bipolar disorder all increase the likelihood of experiencing sleep paralysis. However, having sleep paralysis doesn't mean you have a mental health condition. The relationship works both ways: mental health issues can trigger episodes, and recurrent frightening episodes can worsen anxiety. Addressing mental health often reduces or eliminates sleep paralysis.
Was This Article Helpful?
Yes
No



with Amaha
for Goodon Google Play India

Amaha is equipped to provide care and support for individuals experiencing severe psychological distress, including complex psychiatric disorders and other complex conditions. For those in need of more intensive care and daily support, we are launching an in-patient care facility in Bengaluru soon.
If you or someone you know is experiencing at-risk behaviors or safety concerns, or any other life-threatening crisis or critical mental health situation, contact a helpline or go to the nearest hospital or emergency room. Having a close family member or friend with you for support can be invaluable during this time.
For emergency mental health support, please call the national Tele MANAS helpline at 1-800 891 4416.