
Amaha / / / Signs and Symptoms of Psychosis
ARTICLE | 6 MINS READ
Signs and Symptoms of Psychosis
Published on
9th Jul 2025

Dr Soumya Parameshwaran
MD Psychiatry

When Your Mind Begins to Play Tricks on You
Psychosis is like being caught inside a movie where your mind has taken over the script. It is confusing, terrifying, and usually misunderstood. But here's the reality—psychosis isn't the end of the story. With proper assistance, individuals recover. Completely. Honestly.
Also read this: [Discover psychosis treatment]
What is Psychosis?
Sudarshana Sinha, Senior Psychologist at Amaha, explains, “Psychosis is not a diagnosis—whether you like it or not, it's a symptom.”
It's the brain saying: "Something's not quite right here." Also called a breakdown from reality, psychosis can cause hallucinations (seeing or hearing things that are not there), delusions (firmly held false convictions), and disorganized thoughts or speech.
Psychosis can occur on its own (transient psychotic episodes) or as part of a disorder like schizophrenia, bipolar disorder, major depression, or postpartum illness. And even though it's more common than most are aware of, it's undiagnosed, especially when cultural and gender ideals become barriers.
Read more about the various forms of Psychosis
Symptoms of Psychosis
Psychosis masquerades in many ways. It is not always preceded by grand ideas or unusual or confusing behavior. It sometimes whispers—calling in a person, by him or herself.
In Women
- Psychosis tends to begin later in women, often with changes in hormones such as:
- Postpartum period
- Perimenopause
- Typically misdiagnosed as mood swings or hormonal imbalance
- Possible symptoms:
- Paranoid ideation
- Sudden social withdrawal
- An extremely intense sensation of being watched or controlled
- Postpartum psychosis is a medical emergency and needs treatment urgently
In Men
- Typically develops earlier, late teens to early twenties
- Signs of early warning are:
- Restlessness
- Disturbances of sleep
- Conspiracy-type thinking
- More obvious symptoms:
- Agitation or aggression
- Erratic behavior
- More likely to be dismissed from treatment due to stigma or denial
During Pregnancy
- Antenatal psychosis is rare but important to diagnose
- Symptoms may be:
- Hallucinations related to the baby
- Paranoia about healthcare workers
- Irrational health-related beliefs
- Easily mistaken for anxiety or depression, therefore, early diagnosis is necessary
In Children
- Possible symptoms:
- Talking to invisible friends beyond normal age
- Severe anxiety about common objects or situations
- Strange ideas like "something is controlling my brain"
- Difficult to differentiate from normal imagination—requires professional evaluation
In Adolescents
- Symptoms may develop gradually:
- Decline in studies
- Loss of interest in social contacts
- Developing weird or compulsive interests
- Symptoms may resemble:
- Rebellion
- Depression
- Muttering, performing strange rituals
- Suspicion or distrust of family and friends
In the Indian Context (Cultural Variations)
In India, psychosis sometimes coincides with spirituality. Hallucinations may be perceived as visions of the divine; delusions can be rejected as religious delusions. Families might first seek out religious authorities rather than psychiatrists. Clinic treatment, so delayed by such culturally driven behavior, can prolong suffering. There is also an intense gendered stigma—female psychosis is generally stigmatised as "mad" and relegated, while male psychosis is sometimes considered to be "possessed" or "dangerous." Being attuned to these nuances is critical in culturally responsive diagnosis and treatment.
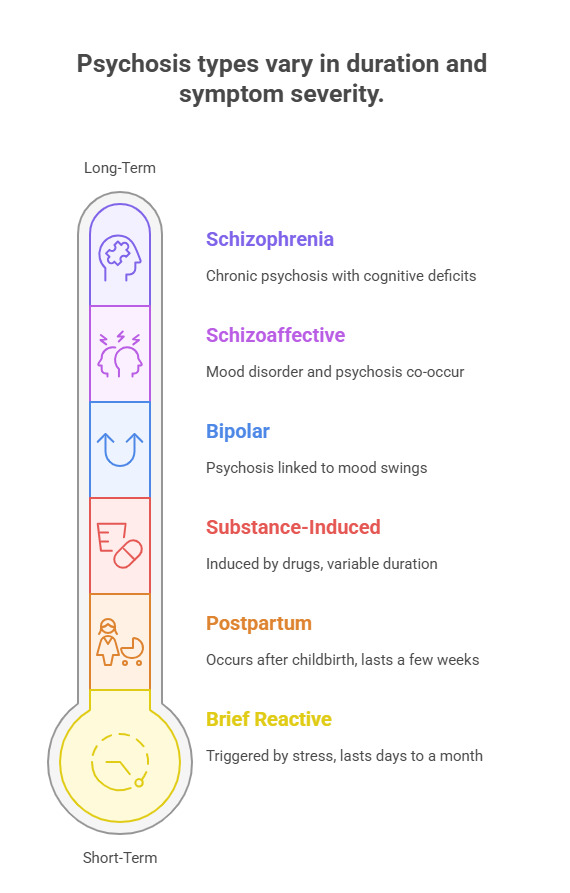
Types of Psychosis and Symptoms
- Brief Reactive Psychosis: Triggered by stress or trauma; symptoms last from a few days to a month.
- Schizophrenia: Long-term psychosis involving hallucinations, delusions, and cognitive deficits.
- Schizoaffective Disorder: Co-occurrence of symptoms of mood disorder and psychosis.
- Bipolar Psychosis: At the extreme mood swings—manic or depressive.
- Postpartum Psychosis: Severe postpartum psychosis after childbirth, typically within two weeks.
- Substance-Induced Psychosis: Induced by drugs like cannabis, LSD, or alcohol withdrawal.
[Want to know what kind of psychosis you may be working with? Have a go at our guided assessment.]
Hidden or Missed Signs of Psychosis
Not all of them are visible. These sneak by:
- Becoming flat or expressionless emotionally.
- Giving strange or irrelevant answers.
- Hyperfixation on odd topics or beliefs.
- Extreme anxiety at the idea of being harmed for no reason.
- Staying alone, avoiding eye contact, or conversation.
- Sudden indifference to showering and dressing properly.
These are warning signs that get written off as "teen angst," "stress," or "being weird." They shouldn't be. Early detection is vital.
Causes and Prognosis
Psychosis is not caused directly. It's a combination of:
- Biological causes: genes, imbalance of neurotransmitters (mainly dopamine).
- Psychological causes: trauma, extreme stress, unresolved grief.
- Medical conditions: brain tumors, infections, epilepsy.
- Substance abuse: cannabis, LSD, methamphetamines, even alcohol.
The prognosis is better than you might think.
With the correct treatment plan and early intervention, many people enter full remission. Delayed treatment, though, makes it harder to recover.
Diagnosis and Assessment
Diagnosis of psychosis includes:
- Clinical interviews (with family and individuals)
- Psychiatric evaluation
- Neuropsychological assessment
- Lab work and imaging (to rule out medical etiology)
It's worth finding an appropriately trained mental health professional—Google is not enough.
[Schedule a session to understand more about this with a licensed therapist today.]
Treatment, Solutions, and Management
There is no one treatment for psychosis. Complete treatment generally includes:
- Antipsychotic medication is used to stabilize.
- Psychotherapy (e.g., CBT or trauma-informed therapy).
- Family therapy to address the home environment.
- Occupational therapy and social rehabilitation in the recovery of function.
- Hospitalisation in acute or severe cases.
- Lifestyle management—habits, eating, sleep, social support—takes its turn too.
Effect of Psychosis
Physical Effect
- Disturbed sleep, fatigue, altered appetite.
- Medication side effects (e.g., weight gain, tremors).
- Risk of chronic disease from health neglect.
Emotional Effect
- Fear, perplexity, shame.
- Loss of self or feeling of worth.
- Social isolation and relationship difficulties.
Living with psychosis (or living with someone who has it) takes strength and knowledge.
Caregivers – Supporting Loved Ones
- Do not argue with delusions. Validate feelings, not erroneous facts.
- Encourage professional help. Be firm but compassionate.
- Educate yourself about the illness. Compassion grows from knowledge.
- Create a calm environment. Stimulate less during episodes.
Take care of your mental health. Caregivers burn out, too.
[Join a caregiver support group]

Worried About Psychosis Symptoms?
Talk to a mental health expert for guidance, support, and next steps.
Frequently Asked Questions
1. Is psychosis identical to schizophrenia?
Not always. Schizophrenia is long-term psychosis, but psychosis may occur with other conditions, as well.
2. Can psychosis disappear on its own?
It may come and go briefly but tends to recur. Treatment does make a difference to long-term survival.
3. Is medication always necessary?
Yes, in more severe and moderate attacks, since it calms the brain and reduces symptoms.
4. Can a person with psychosis lead a normal life?
Yes. Most regain school, work, and relationships if treated early.
5. What should I do if I think someone is experiencing a psychotic episode?
Act calmly. Don't confront. Call a mental health professional as soon as possible
[Reach out to a professional today]
Anuradha Palit, Senior Psychologist at Amaha, assures, “Psychosis may hijack reality, but recovery brings it back. Compassion, awareness, and timely care are the keys. If something feels off—say something. If you’re struggling, don’t hesitate to ask for help.”
Because everyone deserves a mind that feels like home.
Was this article helpful?
Yes
No
If you didn't find what you were looking for, please reach out to us at [email protected] or +912071171501. We're here for you - for anything you might need.



Build a good life for yourself
with Amaha
Best App
for Good
on Google Play India
