
Amaha / / / Bipolar Disorder: Signs and Symptoms
ARTICLE | 8 MINS READ
Bipolar Disorder: Signs and Symptoms
Published on
6th Jun 2025

Dr Divya G Nallur
MD Psychiatry

What is Bipolar Disorder?
Bipolar disorder is a psychiatric condition in which a person experiences recurrent episodes of shifts in mood from extreme highs to extreme lows, which last for several days and make it difficult for them to carry out day-to-day tasks.
The periods of highs are episodes of ‘mania’ characterised by elated or irritable moods, increased energy and activity, and impulsivity. A person experiencing a manic episode is likely to speak rapidly, about various topics, and feel that their thoughts are changing rapidly. They may also develop unrealistic beliefs, start behaving inappropriately, and do reckless things such as spending a lot of money. The manic episodes may vary in severity, and severe symptoms may sometimes require hospitalisation.
Less severe episodes are known as “hypomania”. During a hypomanic episode, a person may feel optimistic and become more productive. Although they may not think that anything is wrong, people around them may notice a change in mood, behaviour and activity levels. Hypomania can also develop into more severe mania or depression without timely treatment.
The periods of lows, called ‘depression’, include feelings of sadness, loss of interest, or hopelessness, along with decreased energy and activity levels. A person experiencing depression will tend to feel tired and find it difficult to concentrate on and enjoy anything. There are often disturbances in sleep and appetite. Depressive episodes can vary in severity, too, with severe episodes often being characterised by suicidal thoughts and impulses.
Dr. Shivam Gupta, a psychiatrist at Amaha, explains, “A diagnosis of bipolar disorder requires at least one episode of mania or hypomania. These episodes can also present with features of both mania and depression simultaneously. This is known as a mixed episode or an episode with mixed features, where individuals might feel sad, empty, or hopeless despite having significant energy. While symptoms typically emerge in early adulthood, they can also begin in childhood or later in middle adulthood”
Every person diagnosed with bipolar disorder has experienced at least one episode of mania or hypomania. An episode can also include symptoms of both mania and depression. In such an episode, people may experience sadness, emptiness, or hopelessness along with a lot of energy. This is called a mixed episode, or an episode with mixed features. Symptoms of bipolar disorder often appear in early adulthood, although they can begin in childhood or middle adulthood, too.
Signs and Symptoms of Bipolar Disorder
It is essential to know that the symptoms of bipolar disorder can vary significantly over time and between individuals.
Here are the primary indicators and symptoms associated with the different mood episodes in bipolar disorder:
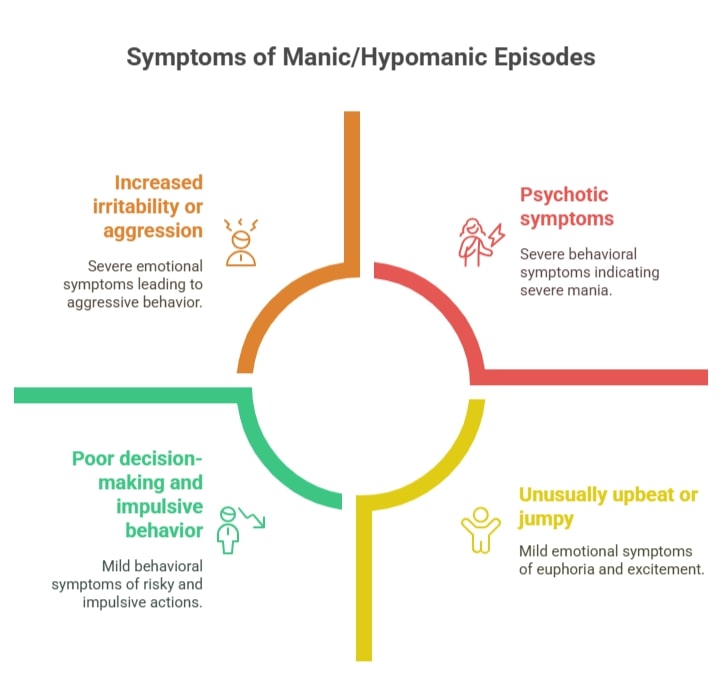
I. Manic/Hypomanic Episodes in Bipolar Disorder
Although mania and hypomania are different types of episodes, they share similar symptoms. Mania is more severe than hypomania and often results in significant issues with daily functioning in areas such as work, school, and relationships. It can also involve a detachment from reality (psychosis), which may require hospitalisation.
Hypomania represents a less intense form of mania. During a manic or hypomanic episode, an individual experiences three or more of the following symptoms for at least a week (or for any duration that necessitates hospitalisation for mania, or at least four days for hypomania):
- Unusually upbeat or jumpy: Feeling excessively happy, excited, or euphoric, often disproportionate to the circumstances.
- Increased activity, energy, or agitation: Feeling restless, having high physical energy, or being unable to remain still.
- Exaggerated sense of well-being and self-confidence: Believing they possess special talents, powers, or importance; inflated self-esteem.
- Decreased need for sleep: Feeling rested and energised after only a few hours of sleep, or not sleeping at all.
- Unusual talkativeness or pressured speech: Speaking rapidly, loudly, and often to the point where others cannot interrupt.
- Racing thoughts or flight of ideas: Rapidly shifting thoughts that make it challenging to follow one’s train of thought.
- Distractibility: Easily diverted by irrelevant stimuli.
- Poor decision-making and impulsive behaviour: Engaging in risky activities without considering the consequences, such as excessive spending or shopping sprees, reckless business investments, or substance misuse (alcohol or drugs).
- Increased goal-directed activity: Taking on multiple new projects or tasks, often simultaneously and without completion.
- Increased irritability or aggression: Becoming easily frustrated, angry, or hostile.
Psychotic symptoms (more common in severe mania): Delusions, which are fixed, false beliefs not based in reality (e.g., believing they are a famous person or have special powers), and hallucinations—perceptions of things that do not exist (e.g., seeing, hearing, smelling, tasting, or feeling things that aren't there).
II. Major Depressive Episodes in Bipolar Disorder (Emotional Lows)
During a depressive episode, an individual experiences five or more of the following symptoms for at least two weeks, significantly disrupting day-to-day activities:
- Depressed mood: Feelings of sadness, emptiness, hopelessness, or tearfulness most of the day, nearly every day. In children and adolescents, this may present as irritability or anger.
- Marked loss of interest or pleasure (anhedonia): No longer enjoying most or all activities once considered pleasurable.
- Significant weight loss or gain, or changes in appetite: Losing or gaining large amounts of weight, or noticeably altering appetite. (In children, failure to gain weight as expected can be a sign.)
- Insomnia or hypersomnia: Trouble sleeping (insomnia) or oversleeping (hypersomnia).
- Psychomotor agitation or retardation: Manifesting restlessness or agitation, or exhibiting slowed movements and speech.
- Fatigue or loss of energy: Feeling constantly tired even after rest, and lacking energy for daily tasks.
- Feelings of worthlessness or excessive guilt: Feeling like a failure or blaming oneself for things beyond one’s control.
- Decreased ability to think, concentrate, or make decisions: Difficulty focusing, remembering, or making even simple choices.
Recurrent thoughts of death or suicide: Thoughts about dying, suicidal ideation, planning suicide, or attempted suicide.
.jpg?alt=media&token=c328a7c3-d6b3-4f13-9a62-fe4bf3a2f94a)
Other Symptoms of Bipolar Disorder:
Mayank Rajput, Senior Consultant Psychologist at Amaha, explains that in bipolar disorder, you might experience mixed features, like feeling incredibly sad but also super energetic and restless all at once, which can be really distressing. And sometimes, anxiety can creep in with your mood, what he calls anxious distress, or a deep, pleasure-robbing sadness known as melancholy.”
- Mixed features: Experiencing symptoms of both mania/hypomania and depression simultaneously (e.g., feeling extremely sad while also being highly energetic and restless). This can be particularly distressing.
- Rapid cycling: Having four or more mood episodes (manic, hypomanic, or depressive) within 12 months.
- Anxious distress: Experiencing symptoms of anxiety and fear of losing control alongside mood episodes.
- Melancholy: Deep sadness with a profound loss of pleasure.
- Seasonal patterns: Mood episodes that tend to arise during specific times of the year.
Is a manic episode the same as a mood swing? Know more.
Signs and symptoms of Bipolar Disorder in women
Women with bipolar disorder often experience:
- Rapid cycling between mood states occurs more frequently.
- Mixed episodes combine mania and depression symptoms simultaneously.
- Mood episodes may correlate with menstrual cycles.
- Symptoms can worsen during perimenopause and menopause.
- Higher rates of thyroid disorders which can complicate diagnosis.
Common symptoms:
- Severe depression with feelings of worthlessness, guilt, and suicidal thoughts.
- Hypomanic episodes that may be less noticeable (elevated mood, increased energy, but still functional).
- Anxiety disorders often co-occur.
- Sleep disturbances and appetite changes.
Signs and Symptoms of Bipolar Disorder in Men
Men usually experience:
- Earlier onset of manic episodes.
- More classic manic symptoms (grandiosity, risk-taking, hyperactivity).
- Less likely to experience mixed episodes.
- Higher rates of substance abuse as a coping mechanism.
- Increased aggression or irritability during manic phases.
- Reckless behaviour like excessive spending, sexual indiscretions, or dangerous driving.
- Work-related problems due to poor judgment during episodes.
Signs and Symptoms of Bipolar Disorder During Pregnancy
Risks and considerations:
- The postpartum period carries a high risk for mood episodes, particularly depression or psychosis.
- Severe mood swings beyond normal pregnancy emotional changes.
- Inability to sleep even when exhausted.
- Extreme anxiety about the pregnancy or the baby's health.
- Racing thoughts or difficulty concentrating.
- Postpartum psychosis (rare but serious): confusion, hallucinations, delusions about the baby.
Read about How Does Bipolar Disorder Affect Relationships
Signs and Symptoms of Bipolar Disorder in Children
Childhood bipolar disorder may include:
- Severe mood swings that are different from normal childhood tantrums.
- Rapid cycling between moods, sometimes within the same day.
- Chronic irritability rather than distinct manic episodes.
- Extreme temper tantrums that are severe and long-lasting.
- Periods of silly, goofy, or elated behaviour.
- Difficulty sleeping or nightmares.
- Separation anxiety or extreme clinginess.
- Complaints of being bored frequently.
- Academic problems and difficulty with peer relationships.
Signs and Symptoms of Bipolar Disorder in Teens
Manic symptoms:
- Unusually high energy and decreased need for sleep.
- Grandiose beliefs about abilities or importance.
- Risky behaviours like sexual activity, substance use, or reckless driving.
- Racing thoughts and rapid speech.
- Extreme mood elevation or irritability.
Depressive symptoms:
- Persistent sadness or hopelessness.
- Loss of interest in activities once enjoyed.
- Significant changes in appetite or weight.
- Thoughts of death or suicide.
- Difficulty concentrating on studies.
Important distinctions:
Adolescent bipolar disorder can be challenging to diagnose. Hence, the Symptoms must be clearly different from normal teenage behaviour. Episodes are typically more severe and longer-lasting than typical adolescent mood swings.
Signs and Symptoms of Bipolar Disorder: Cultural Variations in India
Bipolar disorder in Indian cultural contexts may present with:
- Somatic symptoms (physical complaints) may be more prominent than emotional symptoms.
- Religious or spiritual themes during manic episodes (feeling chosen by God, religious grandiosity).
- Family shame and stigma may delay treatment seeking.
- Symptoms might be attributed to spiritual or supernatural causes initially.
Debunking Common Myths: What You Need to Know About Bipolar Disorder

Not Sure If It’s Sadness or Depression?
It could be more than just sadness. Take this quick assessment to better understand what you're feeling.
Types of Bipolar disorder and their symptoms
Bipolar I
Bipolar I disorder may cause you to experience one or more manic episodes. They usually last for at least seven days. You may feel like being on top of the world or extremely irritated with everything.
While there can be a possibility of depressive episodes in this type, it is not necessarily that everyone experiences its symptoms.
As the changes in your mood can be prominent, the changes can be noticed by your friends, family, and colleagues. If you’re in distress and unable to cope, the symptoms can aggravate and impact your personal and work relationships and productivity levels. Know that talking to a trustworthy companion in times like these can help get you the care and support you need.
Bipolar II
Bipolar II may cause you to experience hypomanic and depressive episodes as opposed to manic episodes. It is often misunderstood as a milder form of bipolar I disorder.
You may consider consulting a mental health professional after your first depressive episode, as it may cause you to feel extreme sadness out of nowhere. The symptoms of hypomania may feel okay to cope with and even aid in academic or work performance.
Past research suggests that bipolar II disorder can lead to other mental health conditions, such as anxiety disorder or substance abuse disorder. These can exacerbate your symptoms of depressive and hypomanic episodes.
Cyclothymic disorder
Cyclothymic disorder or cyclothymia may cause you to experience “mood swings” oscillating from depressive to hypomanic symptoms in shorter, alternating time durations. The symptoms of this disorder are milder than those of the other types.
However, it is still essential to seek the right help and treatment from a mental health practitioner on this. Along with interfering with your daily life, these symptoms also have a chance to develop into bipolar I or bipolar II disorder over time.
Read more about the types of Bipolar Disorder
What causes bipolar disorder?
The causes of bipolar disorder aren’t known yet. However, these factors can potentially increase the chances of developing bipolar disorder.
Environmental Factors
Different environmental conditions can trigger depression and mania in bipolar disorder. Triggers such as inadequate sleep, simultaneous stressful life changes, and lack of physical activity can exacerbate depressive episodes.
On the other hand, mania can be triggered by factors such as loss of a loved one, substance abuse, divorce/break-ups, misuse of prescribed drugs such as antidepressants, job loss, or even changes in sleep patterns.
Genetics and Brain Structure
Research indicates that an imbalance of specific neurotransmitters such as dopamine, serotonin, and norepinephrine is associated with bipolar disorder. These are neurotransmitters that influence your mood.
The possibility of genetic inheritance of bipolar disorder cannot be ruled out while understanding this disorder. Genes can leave you more vulnerable to many mental disorders if they run in your family. According to family and twin studies, you are more likely to have bipolar disorder if your first-degree relatives, such as your parents or siblings, have it.
Childhood Trauma
Childhood trauma is a well-established risk factor for developing bipolar disorder later in life. Various forms of early adverse experiences can increase vulnerability to the condition:
- Physical, emotional, or sexual abuse during childhood can disrupt normal brain development and stress response systems. This can potentially lead to mood instability in adulthood.
- Neglect or inconsistent caregiving can affect the development of emotional regulation skills and create lasting changes in how the brain processes stress.
- Witnessing domestic violence or other traumatic events can have similar effects on developing neural pathways.
- Early loss of a parent through death, abandonment, or prolonged separation can increase risk.
- Chronic family dysfunction or instability during formative years may contribute to the development of mood disorders.
Childhood trauma can lead to persistent changes in cortisol levels and other stress hormones, which may increase susceptibility to mood episodes later in life. It's important to note that while childhood trauma increases risk, it doesn't guarantee someone will develop bipolar disorder. The interplay between genetic vulnerability, environmental factors, and individual resilience all contributes to whether the condition develops.
Stress
The stress hormone cortisol is associated with bipolar disorder. As your stress level increases, the cortisol level of your body goes up too. This causes alterations in how the brain functions and communicates with other parts of the body.
Stressful life events such as the death of a family member or friend, job loss, miscarriage or abortion, being in an abusive relationship, or a highly demanding lifestyle can put you at risk of developing mental disorders.
However, it is often difficult to gauge which stress-inducing events can impact someone, as everyone experiences stress differently. What might be an extremely stressful event for someone might not be something as stressful for you.
It cannot be easy to figure out what causes your mental health condition by yourself. It can help to start a conversation about it with your family, friends, and your therapist and psychiatrist.
Can you get Bipolar Disorder later in life? Know more.
How is Bipolar Disorder Diagnosed?
Diagnosing bipolar disorder is a complicated process that requires careful clinical assessment, as there are no specific blood tests or brain scans that can give a definitive diagnosis of the condition. Mental health professionals rely on detailed evaluation of symptoms, medical history, and standardised diagnostic criteria.
The diagnosis of bipolar disorder follows the criteria established in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which is the standard reference used by mental health professionals. To be diagnosed with bipolar disorder, a person must have experienced at least one episode of mania or hypomania.
Assessment Process for Diagnosing Bipolar Disorder
The expert will start with a clinical interview, which can look like:
- Detailed discussion of current symptoms and their duration.
- Comprehensive medical and psychiatric history.
- Family history of mental health conditions.
- Assessment of functional impairment in work, relationships, or daily activities.
They may also do a mood episode evaluation where they look for specific symptoms during manic/hypomanic episodes.
What are the Diagnostic Challenges for Bipolar Disorder?
Differential Diagnosis
Bipolar disorder must be distinguished from other conditions that can present with similar symptoms:
- Major depressive disorder
- Anxiety disorders
- Attention-deficit/hyperactivity disorder (ADHD)
- Borderline personality disorder
- Substance use disorders
- Medical conditions affecting mood (thyroid disorders, neurological conditions)
Misdiagnosis Issues
Bipolar disorder is often misdiagnosed because many people seek help during depressive episodes rather than manic/hypomanic episodes. Hypomanic episodes may be overlooked or misinterpreted as periods of high productivity. The symptoms might also overlap with other mental health conditions. There could also be cases of co-occurring conditions, which can complicate the diagnostic procedure.
How OCD and Bipolar Disorder Are Connected? Read here.
Diagnostic Tools for Bipolar Disorder
Mood Tracking
Mood charts or journals to track patterns over time
Documentation of sleep patterns, energy levels, and behaviour changes
Identification of potential triggers or patterns
Standardised Assessments
- Mood Disorder Questionnaire (MDQ)
- Bipolar Spectrum Diagnostic Scale (BSDS)
- Young Mania Rating Scale (YMRS)
- Hamilton Depression Rating Scale
Our psychiatrist, Dr Divya G Nallur talks about diagnosing bipolar disorder, “It is important to note that an accurate diagnosis is crucial for bipolar disorder, as treatment approaches differ between bipolar disorder and other mood disorders. If misdiagnosed (with depression), certain antidepressants can trigger manic episodes in people with bipolar disorder.”
How does Bipolar Disorder impact Everyday Life? Read here.
Bipolar Disorder: How to navigate as a Caregiver?
Being a caregiver for someone with bipolar disorder can be both rewarding and challenging. Your support can make a significant difference in your loved one's recovery and quality of life, but it's important to approach caregiving with knowledge, compassion, and strategies for taking care of your well-being.
How can you provide support to someone with bipolar disorder?
- Show Compassion and Acceptance: Make sure they feel accepted and let them know it’s going to be okay.
- Listen empathetically: Validate their feelings and experiences when they voice them. Avoid trying to "fix" them or their emotions.
- Communicate Effectively: Be calm and use non-confrontational language.
Creating Emergency Plans
It is important to have things ready during an emergency. Work with your loved one to create plans for managing future episodes. Identify early warning signs specific to them and list coping strategies that have worked before. Know who to contact in emergencies and how to access emergency services.
Taking Care of Yourself
“You can’t pour from an empty cup.”
Research shows that nearly 70% of caregivers reported being distressed by how bipolar disorder has affected their own life and emotional well-being.
Understanding caregiver burnout
Being a caregiver can often lead to burnout, where one feels constantly exhausted or overwhelmed. You may lose interest in activities you once enjoyed, become irritable or resentful. You may even feel hopeless about your loved one's condition.
During such instances, it’s important to cope with it by setting boundaries and taking care of yourself. Decide what support you can realistically provide. Communicate your boundaries. Take care of your physical health and maintain relationships with friends and family outside of caregiving with regular breaks from caregiving responsibilities.
While your support is crucial and valued, it's important to remember that you cannot cure or control your loved one's bipolar disorder.

Talk to a Coach
Feeling stuck or overwhelmed? Get support and clarity in a free call with one of our mental health experts.
FAQS
1. What is the first red flag of bipolar disorder?
The first red flag in bipolar disorder is elevated mood, activity, or energy known as mania or hypomania. This is a shift from typical behavior.
2. Is bipolar disorder curable?
While bipolar disorder is not curable, it is highly manageable with the right resources and support.
3. At what age does bipolar disorder start?
Symptoms of bipolar disorder typically show in the teenage years or early 20s.
4. Can a person with bipolar disorder live a normal life?
A person with bipolar disorder can live a relatively normal life with effective support and symptom management.
5. Is bipolar disorder genetic?
Yes, bipolar disorder has a strong genetic basis, with multiple genes involved. Read more here.
Was This Article Helpful?
Yes
No



Build a good life for yourself
with Amaha
Best App
for Good
on Google Play India

Amaha is equipped to provide care and support for individuals experiencing severe psychological distress, including complex psychiatric disorders and other complex conditions. For those in need of more intensive care and daily support, we are launching an in-patient care facility in Bengaluru soon.
If you or someone you know is experiencing at-risk behaviors or safety concerns, or any other life-threatening crisis or critical mental health situation, contact a helpline or go to the nearest hospital or emergency room. Having a close family member or friend with you for support can be invaluable during this time.
For emergency mental health support, please call the national Tele MANAS helpline at 1-800 891 4416.